Publications
The Center exists in part to create original evidence and information that support and advance conversations around professionalism, value, and other health care issues.
READ about scientific publications, briefs, and reports emerging from the Center and its collaborators below.
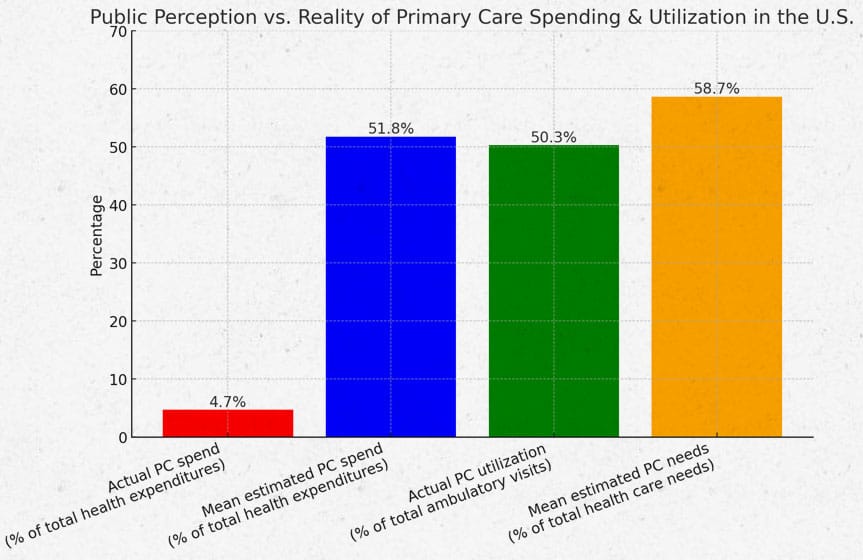
The General Public Vastly Overestimates Primary Care Spending in the United States
- Melissa Ma
Submitted on: March, 2025
This study assessed public perceptions of US primary care spending. An online survey was conducted using SurveyMonkey Audience (Symphony Technology Group), achieving a sample of 1,135 adult respondents reflective of the demographic distribution of the US adult population. Respondents’ mean estimate of the percentage of US health care spending funding primary care was 51.8% (SD 24.8, interquartile range [IQR] 40). Respondents’ mean estimate of the percentage of health care needs addressed by primary care was 58.7% (SD 22.2, IQR 28.5) These results reveal a tremendous disparity between current levels of primary care spending (4.7%) and public perceptions of primary care expenditure and value.
Exploring Community-Based Residency Programs in High-Need Black Counties
- Michael Topmiller, PhD
Submitted on: February, 2025
Primary care physician (PCP) shortages and uneven geographic distribution are well-documented. Black populations have less access to primary care and worse health outcomes, with a lack of provider-patient racial concordance playing a role. Addressing these disparities requires targeted approaches that produce more Black PCPs in high-need areas, including expanding community-based residency programs (CBRPs), which are more likely to produce physicians in high-need areas. This research explores the relationship between high-need Black counties and the location of CBRPs.
Evaluating primary care expenditure in Australia: the Primary Care Spend (PC Spend) model
- Michael Wright
Submitted on: January, 2025
The application of the Primary Care Spend model to Australian data provides a more nuanced analysis of expenditure for primary health care than routine health expenditure reports. Its output could be used to inform targets for spending on different tiers, types, and locations of primary care, especially comprehensive and other high value primary care services, and to monitor progress toward these targets.
Read More

