Happy Fall from the CPV!
We have been quite busy and cannot wait to share all our latest happenings!
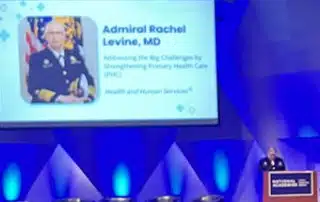
Primary Care International Conference
The Essential Role of Primary Health Care for Health Security and Securing Health
Background/Overview
This conference took place nearly 5 years after the Declaration of Astana and focused on advancing Primary Health Care in developed and developing countries as a priority for national health security and securing the health of people around the world. This conference follows up on the National Academy of Medicine (NAM) Primary Care report’s 3rd stated task: to inform primary care systems around the world. We thoughtfully crafted a two-day international conference, featuring prominent primary health care (PHC) leaders from both high-income and low- and middle-income countries, who would share their innovative approaches and challenges in implementing PHC since the Declaration of Astana. Our goal was to seize a policy window created by the HHS Primary Health Care Action Plan to foster and unite strategic coordination of effort across U.S. health agencies, paving the way for significant improvements in health.
Learn more about the conference in an interview with Dr. Bob Phillips and Dr. Lauren Hughes, HERE.
Attendance: 20 Countries Represented
A total of 170 people attended from more than 20 countries, and the following government agencies/organizations:


Campbell Cook
June-August 2023 Visiting Scholar
During my summer at the center, I worked on two projects and helped with the logistics of the Primary Care International Conference. The first project I started working on focuses on understanding physician perspectives on the state of self-regulation and what role self-regulating organizations like the specialty board should play in maintaining standards of professionalism. I have completed an initial review of the literature and am currently working with Annie on facilitating interviews on the topic. After the interviews, I will be assisting with thematic coding. I also have been working on a project with Annie, Andrew, and Dave seeking to identify and discuss important competencies for rural primary care practice. I helped Annie facilitate some of those interviews as well and have been leading the screening phase of a scoping review for the project. The screening phase is nearly complete, and it is our plan to publish papers based on the interviews and scoping review. For the conference, I helped prepare the name tags and signage, checked attendees in, helped usher people, and took notes.

Annalise Bickley
January-July 2023 Visiting Scholar
With my time at the Center for Professionalism and Value in Health Care, I had the opportunity to utilize qualitative research and be a part of the planning and production of the international conference The Essential Role of Primary Health Care for Health Security and Securing Health. My research was conducted across multiple research databases including PUBMED, the Lancet, and Google Scholar. From this research, I constructed an annotated bibliography on Primary Care and Public Health in Developing and Developed Countries. My role with the conference allowed me to help with the organization and coordination of attendees, RSVPs, speakers, and questions leading up to the event alongside Mikel Severson. Throughout the conference I was an active point of contact and coordination for attendees, set up and take down the conference, and was an active participant. I was able to improve my communication, collaborative, and networking skills, along with gaining valuable professional experience and continuing to grow my interest for public health in the process.

Jenna DeLucca
June-July 2023 Visiting Scholar
This summer I spent two months in Washington, DC working at the CPV. During my time here I worked on multiple projects. I had four major projects to work on during my time in DC, including two of which are still ongoing while I am home and when I return to school. I helped the Lexington PRIME team connect with state Medicaid agencies for a new CMS program, Making Care Primary. I also worked extensively on the PHC International Conference, creating all the slides and then running the slides during the conference for both days. I am still in the beginning stages of moving my research forward on how Maryland practices enrolled in the Maryland Primary Care Program (MDPCP) are using the money they receive from the state, called HEART payments, to address patients’ health-related social needs. I am conducting a qualitative study on how these practices use the additional $110 per qualified patient they receive from the state and how the PRIME Registry and PHATE specifically, is used and if these tools influence where they decide to allocate their HEART payments. Finally, I am also in the process of updating the annotated bibliography “Teaching Population Health” from 2017 using the same methods and criteria, but integrating articles that have been published since this paper was initially written.

Welcome to the CPV Team, Dr. Marci Nielsen!
Dr. Nielsen has joined the CPV Team, as the Senior Consultant for Policy and Public Engagement. With three decades of experience in global, federal, state, association, and academic leadership roles, Marci Nielsen, PhD, MPH consults with organizations to advance policy, research, and networking strategies to improve health – ‘Pro Re Nata” (PolicyPRN Consulting, LLC).
A former Peace Corps volunteer and public health researcher, Marci served as health legislative assistant for U.S. Senator Bob Kerrey-NE, and later as health lobbyist and deputy director of legislation at the AFL-CIO (American Federation of Labor and Congress of Industrial Organizations) in Washington, DC. She taught graduate and medical students as a faculty member at the University of Kansas Medical Center (KUMC), later serving as vice chancellor of public affairs. Appointed by Governor Kathleen Sebelius, Marci directed the Kansas Health Policy Authority (responsible for Medicaid, CHIP, the State Employee Health Plan, and health IT) for three years. For five years she served as CEO of the Patient-Centered Primary Care Collaborative, a national multi-sector association advocating for advanced primary care. In 2017, she launched PolicyPRN Consulting LLC and subsequently joined one of her full-time clients, the Government Employee Health Association (GEHA), as vice president for policy and strategy. When COVID-19 hit, Marci returned to state government service working as chief advisor for COVID-19 coordination for Kansas Governor Laura Kelly. She led Kansas’ unified testing strategy, stakeholder engagement, and vaccine roll-out. She then joined a global civil society organization founded by former CDC Director Dr. Tom Frieden to help lead U.S. advocacy efforts to invest in global and U.S. public health and primary health care before returning to health consulting full time in 2023.
Marci has a PhD from Johns Hopkins School of Public Health, an MPH from George Washington University, and a BS in biology and psychology from Briar Cliff College. She has served on several non-profit health boards (National Academy for State Policy, the American Board of Family Medicine, Collaborative Family Health Association), various state and federal advisory committees, and co-edited the Policy Section of the Journal “Families, Systems, & Health” (a journal of the American Psychology Association). She is currently a member of the Board of Trustees for the American Academy of Family Physicians (AAFP) Foundation.

Dr. Kevin Grumbach
CPV/George Washington University Fellowship: 2023-2024
Our fellow candidate for this academic year was accepted to the White House Fellowship instead, so we have developed an alternative plan with George Washington University. Dr. Kevin Grumbach has agreed to serve the Family Medicine Division and University as a part-time consultant on the development of a family medicine department and will join the CPV for policy-focused work. Dr. Grumbach is a family physician, academic and advocate for single-payer health insurance. He is the past-chair of the Department of Family and Community Medicine at the University of California, San Francisco.
COVID-19 Research

Dr. Nathaniel Hendrix
Senior Research Scientist
Dr. Nathaniel Hendrix’s article, Influence of Prior SARS-CoV-2 Infection on COVID-19 Severity: Evidence from the National COVID Cohort Collaborative has been in the news, including a mention in a CNN article, and for all you daytime soap opera and Dallas fans, Nathaniel’s article was also retweeted by Morgan Fairchild!
Dr. Nathaniel Hendrix
Senior Research Scientist
Dr. Nathaniel Hendrix’s article, Influence of Prior SARS-CoV-2 Infection on COVID-19 Severity: Evidence from the National COVID Cohort Collaborative has been in the news, including a mention in a CNN article, and for all you daytime soap opera and Dallas fans, Nathaniel’s article was also retweeted by Morgan Fairchild!
The Core Quality Measures Collaborative (CQMC) Recently Announced That ABFM’s Continuity of Care and Person-Centered Primary Care measures Will Join the Core Measure Set
Recently, the CQMC announced updates to eight of its core measure sets – which include ABFM’s Continuity of Care and Person-Centered Primary Care measures. This means that health plans across the country should adopt these measures to improve patient care. The CQMC is public-private partnership between AHIP and the Centers for Medicare and Medicaid Services, representing over 75 consumer groups, medical associations, health insurance providers, purchasers, and other quality stakeholders, all working together to develop and recommend core sets of measures by clinical area to assess and improve the quality of health care in America.
Person-centered and continuous doctor-patient relationships are essential to primary care. Reams of evidence show that these relationships lead to lower costs, higher patient satisfaction, increased professional satisfaction for physicians, burnout prevention, and better health outcomes in a wide range of chronic disease areas. These measures are critical to providing more equitable care and improving health outcomes.
New Survey Data of ABFM Diplomates Highlights the Critical Importance of Doctor-Patient Relationships in Primary Care
The survey from the ABFM showed that nearly all family medicine physicians who responded (99.7%) agree that continuous patient-doctor relationships over time translate into optimal patient care, improved diagnoses, and better patient outcomes. Further, continuous patient-doctor relationships are backed by substantial evidence showing that these relationships lead to lower costs, higher patient satisfaction, increased professional satisfaction for physicians, burnout prevention, and better health outcomes in a wide range of chronic disease areas. The survey is the first of its kind, showing that nearly 8 in 10 (79%) family doctors believe that continuity of doctor-patient relationships is a better measure of their work as a primary care professional than most other existing quality measures that are used by health plans to assess their performance. The survey comes at a time when the Core Quality Measures Collaborative (CQMC) just announced that ABFM’s Continuity of Care and Person-Centered Primary Care measures would be included in their “core measure set” – a group of scientifically sound measures that should be adopted by public and private sector health plans and used for payment and performance improvement. A formal press release from AHIP and CMS was released in August 2023 CQMC Announces Updates to Eight Core Measure Sets – AHIP.